The Influence Of HGH on Bone Mineral Density And Bone Health
When used correctly, Human Growth Hormone (HGH) can deliver many benefits: skyrocketing energy, increased muscle tone, melting dangerous fat, easing joint aches and pains, sharpening mental focus, and promoting a good night's sleep.
But there is another benefit of HGH replacement therapy that is often overlooked: the protection HGH provides to your bones.
Osteoporosis Guideline: Diagnosis and Treatment
We often hear about the dangers of osteoporosis, but we rarely hear the disease explained. From a linguistic standpoint, Osteoporosis means porous bones. The disease is highly associated with an increased risk of bone breaks and fractures. As men and women (especially women) 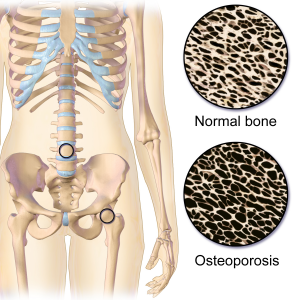 grow older, the risk for severe damage to the hips and spinal column can result.
grow older, the risk for severe damage to the hips and spinal column can result.
Hip fractures are one of the single most dangerous breaks that can occur to the human body, and these fractures are associated with a significantly increased mortality risk.
Hip Fractures and Increased Mortality A recent study released by the University of Pennsylvania Medical School shows that women who have recently experienced a hip fracture have over twice the mortality rate of female patients who did not.
Patients who did not experience these fractures had an annual mortality rate of 8.4%, whereas those who experienced a hip fracture had a mortality rate of 16.9%.
This mortality rate was adjusted to account for confounding health factors and averaged for general bone density. Osteoporosis is one of the primary culprits which lead to bone fractures, and Human Growth Hormone has been shown to reduce the risk of these devastating breaks through HGH Injections.
How is Osteoporosis Diagnosed? The World Health Organization officially designates osteoporosis as a Mineral Bone Density greater than 2.5 Standard Deviations lower than the average bone density of young and healthy individuals with normal bone health.
The Three Forms of Osteoporosis
Primary Type 1 Osteoporosis: Primary Type One Osteoporosis usually strikes in women after menopause. This form of osteoporosis occurs in females at a greater rate than in males. Women are diagnosed with Primary Type 1 Osteoporosis six times more often than males. This form of Osteoporosis develops slowly after menopause (or Andropause in men) and generally takes ten to fifteen years to become diagnosable.
Linked to Hypogonadism (Sexual Hormone Deficiency) This type of osteoporosis is directly linked to sex hormone deficiency in both sexes. In women, Estrogen is vitally essential to maintain bone health properly. In males, proper Testosterone levels are equally as important. Women are diagnosed far more often than their male counterparts that Menopause represents a much more marked hormonal contrast than andropause.
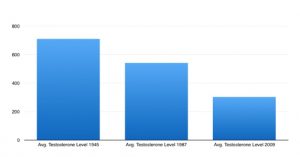
What is Andropause? Andropause is the male form of menopause. During Andropause, Testosterone levels decline over time, leading to a highly symptomatic form of Testosterone Hormone Deficiency. Testosterone levels start to decline around the age of thirty, which produces more and more problems as Testosterone Levels in the body become increasingly meager.
When does Andropause Lead to Osteoporosis? Although men continue to produce Testosterone throughout their lifespan, by the time men reach their fifties and sixties, their bones start to become at risk for osteoporosis. A number of other symptoms of Testosterone Deficiency can start to appear much earlier, however. Muscle strength starts to deteriorate in the late thirties and early forties.
Metabolism rates can drop significantly by the mid-thirties, leading to increased weight gain exacerbated by a sedentary lifestyle.
Why does Osteoporosis Take so Long to become Symptomatic? The reason why bone health takes much longer to decline is because of the natural resiliency of the skeletal system. The bones have such a high rate of structural integrity that the effects of hormonal deficiency take much longer to produce symptoms; but, at the same time, the results of the deficiency are just as, if not more, dangerous to the long-term health of the male and female body.
High-Turnover Osteoporosis Primary Type One Osteoporosis is often referred to as high-turnover osteoporosis because trabecular bone tissue degrades rapidly as the disease approaches a symptomatic point. Trabecular bone tissue is also referred to as Spongy Bone or Cancellous Bone. This type of bone tissue has a large surface area because of its natural porous structure.
Cancellous bone degrades quickly due to osteoporosis because the already porous bone becomes so structurally degraded that it becomes highly prone to fractures and breakage.
This type of bone tissue is mainly located near the edges of bones, near the cartilage in the areas where the bones make contact with one another. Trabecular bone tissue is incredibly densely allocated in the areas of the wrist and the spine. For this reason, patients suffering from osteoporosis are much more at risk for carpal tunnel syndrome and spinal fractures.
Primary Type 2 Osteoporosis Primary Type Two Osteoporosis is the form of the disease that most men and women associate with Osteoporosis because of its relationship with hip fractures. Type Two also affects women at a higher rate than men.
This form is twice as common in females as males, so it is more of a risk for men than Primary Type One Osteoporosis. This manifestation of the disorder usually begins to appear when adults enter their seventies and eighties.
Primary Type 2 Osteoporosis is often, but not necessarily, related to Estrogen and Testosterone Production, but rather Calcium Deficiency and Vitamin-D  deficiency, the two most highly associated with bone health and structural integrity. There is also significant evidence that this disorder is linked to higher activity in the Parathyroid gland associated with aging.
deficiency, the two most highly associated with bone health and structural integrity. There is also significant evidence that this disorder is linked to higher activity in the Parathyroid gland associated with aging.
What is Primary Type Two Osteoporosis? This type of Osteoporosis occurs when the bones have degraded to a point at which even the cortical bones begin to break down. Cortical bones are the strong hard casings of the bone which protect the functional interior bone and support the body's weight throughout the day-to-day function.
Primary Type Two Osteoporosis is associated with a much higher likelihood of breaks of the long arm and leg bones and the hips.
The Hips are Particularly Vulnerable to Breakage Hips are highly susceptible to this form of osteoporosis because, although these bones are quite thick and structurally strong, they are still thinner than many of the other bones of the body. In addition, the hip bones take on an extraordinary amount of stress because of their central, pivotal location in the body.
Another reason that the hip bones are highly at risk for fracture and breakage is because seemingly innocuous falls become incredibly hazardous as Osteoporosis worsens. The hip bone is most likely to take most of the damage in this type of fall.
One slip and the hip bone could fracture or even shatter. As a result, depending on the fall's force and the disease's progression.
Type One and Type Two Osteoporosis Are Unique Disorders Although Primary Type One and Primary Type Two Osteoporosis are considered separate disorders, and Type Two can sometimes occur even in the absence of Type One Osteoporosis, Type Two Osteoporosis can also be the result of a progression of Type One. Over time, the structure of the hips and spinal column degrades to a point that these thicker bones also begin to show symptoms.
These bones take much longer to show signs of wear because the cortical bones are much more compact. Dangerously low levels of Bone Mineral Density take longer to result in fractures and breaks. This is one reason why Type One Primary Osteoporosis is most common between the ages of 55 and 70, and Type Two is more common among patients 70 and older type Two affects bones that are more structurally sound.
Secondary Osteoporosis Secondary Osteoporosis results from factors outside of general nutrition, parathyroid activity, and sex-hormone activity. In healthy men and women, the bone tissue is constantly restructuring itself, replacing aging cells to maintain optimal bone strength. To provide an example, this is why after you break a bone when you are young, the bone can rebuild and even become stronger than it was before. Have you ever broken a bone?
Run your hand along the broken bone area, and you will likely feel that this area of bone is slightly thicker than the bone tissue surrounding it. This is because the body reacted to the damage by making the bone stronger than before.
Bone Remodelling and Osteoporosis The process of natural bone restructuring is known as remodeling. The skeletal system is just like a road or a building. Stress wears on the bones the same way it wears on the tresses of a house or the concrete foundation of a street. Eventually, the street needs to be repaved, and the support structure of a building has to be inspected and maintained. In the body, the bones go through the remodeling process to keep bones constantly in a state of optimal strength.
Bone Formation and Bone Resorption This natural remodeling process results from a delicate balance of two internal processes. The first 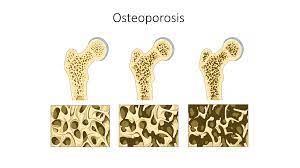 process is known as Bone Formation. In the process of Bone Formation, the bone tissue pulls calcium from the bloodstream to use it to build and strengthen the bones.
process is known as Bone Formation. In the process of Bone Formation, the bone tissue pulls calcium from the bloodstream to use it to build and strengthen the bones.
The cells which perform the task of rebuilding the bones are known as osteoblasts. These cells use enzymes and chemical reactions to pull the calcium from the blood, mineralizing it and affixing it to the bones to strengthen them.
The second process is known as Bone Resorption. Bone Resorption is the process by which older bone cells are broken down and turned back into parts that the osteoblasts can use to create healthy new bone cells.
Osteoblasts and osteoclasts function through the influence of hormones known as Paracrine Signallers. Over a year, ten percent of bone tissue goes through remodeling. When balanced, it is a slow yet effective process for maintaining bone health.
Bone Turnover Rate and Osteoporosis Diagnosis The mathematical formula for maintaining Bone Remodelling is known as the Bone Turnover Rate. A healthy Bone Turnover Rate would be a point at which bone tissue is replaced efficiently, discarding or recycling old tissues and maintaining a constant level of bone strength.
Osteoporosis occurs when the Bone Turnover Rate gets out of balance, and the bone tissue is not recycled and remodeled at the rate that the bone is either degraded by osteoclasts or naturally breaks down due to the aging of the bone cell. Secondary osteoporosis results from osteoclasts that break down bones faster than osteoblasts can rebuild them, causing them to break down and become porous.
Causes of Secondary Osteoporosis Secondary Osteoporosis can be the result of a number of issues related to hormone imbalance, including:
Hyperparathyroidism The parathyroid glands have a single purpose. They are responsible for regulating calcium balance throughout the human body. Hyperparathyroidism is a common cause of Secondary Osteoporosis.
The Parathyroid Glands release a hormone known as Parathyroid Hormone, abbreviated PTH, into the bloodstream. Hyperparathyroidism causes the body to constantly send messages to the bones demanding that they release calcium into the bloodstream. This prevents the Osteoblasts from being able to produce new bone at the rate that bone is being degraded, leading to osteoporosis over time.
Hyperparathyroidism also leads to a constant elevation of calcium in the bloodstream because the body cannot excrete the calcium released by the bones quickly enough. The kidneys are also overworked, often leading to kidney stones. Kidney stones are simply calcium deposits that form in the kidneys.
If they grow large enough, they can block the path of excretion, causing great pain. Hyperparathyroidism is usually the result of a parathyroid tumor which causes the organ to release PTH in overdrive. This form of Osteoporosis can strike men, women, and children of all ages and will not be cured until the tumor is removed or the disorder is otherwise corrected.
Hyperthyroidism Overactive Thyroid Glands prevent the body from storing phosphorus and calcium properly. Hyperthyroidism causes bone turnover at an escalated pace, and the osteoblasts can no longer work fast enough to rebuild bone.
Hyperthyroidism also causes the body to pull calcium and phosphorus out of the bones and diet, where they are excreted through stool or urination. The osteoclasts break down old bone, and the excess materials are pulled into the bloodstream.
This disorder becomes even more problematic when combined with Estrogen Deficiency, Testosterone Deficiency, or Human Growth Hormone Deficiency because the two primary keys to bone health are proper nutrition and proper hormone balance.
Hyperthyroidism often causes an issue known as hypercalcemia, where the bloodstream is flooded with excess calcium. Calcium levels in these patients can be as much as 25% above average.
Diabetes Insulin desensitization results in dangerous levels of blood sugar. Diabetes has been correlated with reduced bone density, resulting in an increased incidence of osteoporosis. Patients who suffer from Diabetes have reported a history of bone fractures at a rate over 12 times higher than their counterparts without diabetes. One reason that Diabetes may affect osteoporosis is that high blood sugar levels in the body reduce the production of Human Growth Hormone by the pituitary gland.
This reduction of HGH production leads to a cascade of issues associated with HGH Deficiency, and Osteoporosis is one of the most dangerous symptoms of Hypopituitarism. Human Growth Hormone directly contributes to bone health because Endogenous Growth Hormone is converted into one of the primary Paracrine Signallers known as Insulin-like Growth Factor One.
IGF-1 plays a direct role in the proper function of Osteoblasts, and when those cells do not function optimally, the bone begins to degrade.
Cushing's Syndrome Cushings Syndrome is symptoms resulting from long-term excess cortisol levels in the body. Cushing's Syndrome is an asymptomatic form of hypercortisolism. Hypercortisolism is simply defined as excess levels of cortisol. Cushing's Syndrome leads to bone issues in a manner that is similar to Diabetes, although other symptoms of the two diseases are incredibly different.
Long-term hypercortisolism leads to a significant decrease in the functional capacity of the osteoblasts. Cushing's Syndrome is common among football players and other professional athletes because of the use of Cortisol as an anti-inflammatory and pain-relieving agent.
Although Cortisol is the body's natural response to pain and inflammation, it also hinders the body's ability to produce Testosterone, Estrogen, and other hormones related to long-term health. Hypercortisolism also leads to symptoms of Testosterone Deficiency, such as mood disorders, hypertension, diabetes, and muscle atrophy, in addition to osteoporosis.
Non-hormone Related causes of Secondary Osteoporosis include:
Metastatic Bone Disease - This stage of cancer in which cancer cells spread throughout the body after being released into the bloodstream. There are multiple reasons why this causes osteoporosis, depending upon the body's regions.
Leukemia This causes White Blood Cells to be generated at a highly escalated rate. This incredible increase in white blood cell production interferes with the proper function of osteoblasts, preventing them from restoring bone calcium and phosphorus levels. The bone marrow produces white blood cells in the same region where osteoblasts primarily operate, and the proliferation crowds out the osteoblasts.
Multiple Myeloma is a stage of bone cancer where multiple tumors grow throughout bone and bone marrow tissue. Multiple Myeloma causes the bone marrow to produce plasma at an uncontrollable rate, preventing the bones from producing other vital cellular organs that regulate Bone Remodelling.
Thalassemia This is a hereditary form of anemia in which the body does not produce enough red blood cells for the body to function optimally. This causes symptoms of osteoporosis and osteopenia to occur early in life because the osteoblasts cannot build bone as fast as it is broken down. Thalassemia is also associated with Human Growth Hormone and IGF-1 Deficiency.
Case Study: Osteoporosis and HGH Deficiency
A study by Dr. Christian Wuster is related to the effects of paracrine signals on the maintenance of the cycle of bone remodeling.
Dr. Christian Wuster is a member of the Department of Internal Medicine, Internal Endocrinology, and Metabolism at the Heidelberg University Medical Clinic in Germany. A recent study released by him and his associates at the university provided evidence that HGH Deficiency is associated with a reduction in bone mass that causes an increased rate of osteoporosis and vertebral fracture.
Children who suffer from juvenile Growth Hormone Deficiency struggle with inferior bone mineralization due to their deficiency. Untreated, this prevents these juvenile patients from experiencing the growth associated with puberty. Osteoporosis can also occur as a result.
Bone Turnover Rates Briefly Decline Because of HGH Treatments When utilizing Human Growth Hormone Replacement Therapy for patients with Growth Hormone Deficiency, the initial rate at which bone turnover occurs is elevated for around the first six months to a year of treatment. This is because the system of bone remodeling is in the process of returning to optimal function.
Before osteoblasts can do their jobs to total capacity, the osteoclasts must play a role in feeding recyclable materials for the process to occur at an optimal rate. After this point, the rate of bone turnover reaches a balanced point, and the bones begin to strengthen as a result.
Research involving individuals with acromegaly shows that dense bone mass increases due to Human Growth Hormone Injections. The therapy does not affect the spongy bones in patients who do not suffer from Hypopituitarism. In patients who suffer from hypopituitarism, trabecular spongy bone mass decreases in area. Although there is a decrease, the trabecular bones have increased mineral content, and their surface area increases.
In Cancellous Tissue, Greater Density Does Not Always Mean Greater Strength This means that although total bone mass decreases slightly, the structural integrity of the bones increases because the bone is healthier. After all, the bone is more optimally composed. One issue with osteoporosis in the trabecular bones is that they are not remodeled efficiently. This means that bone tissue begins to break down and weaken and lose its mineral content even though overall mass remains stable or increases slightly.
This data regarding trabecular mineral content was previously shown to be true in laboratory animal studies involving rats. HGH Replacement Therapy can be used to maintain bone health, maturation, and Mineralization in patients who suffer from Juvenile-Onset Growth Hormone Disorder.
Until juvenile patient achieves their final adult height, they are injected with high doses of Human Growth Hormone to simulate the natural process of puberty, which is caused by the endogenous production of high levels of Human Growth Hormone by the pituitary gland.
process of puberty, which is caused by the endogenous production of high levels of Human Growth Hormone by the pituitary gland.
Adult HGH Hormone Replacement Should Emulate Normal Adult HGH Secretion After the patient reaches Final Adult Height, smaller doses of Human Growth Hormone should be used to emulate HGH levels in the body during adulthood. Although Human Growth Hormone is known primarily for its function in the growth spurt of puberty, it is also vitally important to overall health throughout the lifespan.
HGH Balance is Vitally Important to a Healthy Life Although Dr. Wusters's study shows the importance of Human Growth Hormone to prevent Osteoporosis, Human Growth Hormone is also essential in maintaining a number of other vital functions as well.
HGH encourages a healthy Body Mass Index by facilitating the breakdown of adipose fat tissue. Human Growth Hormone increases muscle mass by increasing the energy and nutrients available to the muscles during exercise. These are just the three most obvious changes associated with Human Growth Hormone Replacement Therapy.
Female Osteoporosis often Caused By Pituitary Imbalance In female patients who suffer from Osteoporosis, Wuster finds that the Growth Hormone/Insulin-like Growth Factor 1 Axis is disturbed and incorrectly regulated, which results in a reduction of bone strength.
Post-Menopausal osteoporosis patients have been shown to have low levels of IGF-1 and IGFBP-3, which lead researchers to conclude that osteoporosis is caused at least partly by a reduction in Growth Hormone Secretion or some other issue involving the Hypothalamic-Pituitary Axis which prevents IGF-1 and IGFBP-3 from being produced correctly.
IGFBP-3 is Insulin-like Growth Factor-Binding Protein Three. The issues caused by this exceed those caused by general hormone decline known as Somatopause. Early-onset Somatopause could present issues in some patients who suffer from arthritis; 24-hour Growth Hormone Profiles do not change among patients who suffer from osteoarthritis and osteoporosis.
What We've Learned: Wuster, Osteoporosis, and HGH Wusters study provide evidence that there are benefits to utilizing Human Growth Hormone shots as a treatment for Osteoporosis. This is because Human Growth Hormone improves bone mineral density and helps sustain a healthy balance of osteoblast-osteoclast function leading to more efficient Bone Remodelling.
These benefits will significantly impact late post-menopausal patients suffering from Primary Type-Two Osteoporosis because the dangers of cortical bone and spinal column fractures become very high during this period. Human Growth Hormone Replacement Therapy may also prevent Osteoporosis and can significantly alleviate the symptoms of Primary Type-One Osteoporosis.
Information regarding Dr. Wuster's study was acquired from the National Library of Medicine.
Osteoporosis and Hypogonadism Bone health are primarily regulated by sex hormones in both males and females. These Hormones play a role alongside Human Growth Hormone in producing Final Adult Height in pediatric patients. In adults, androgens also play an essential role in the skeletal system's maintenance. Significant research correlates deficiencies in Estrogen, Testosterone, and other Sex Hormones with Osteoporosis and other bone disorders.
Estrogen hormones play a vital role in bone health. The male body can convert Testosterone into Estrogen to maintain bone health, although excess estrogen production is very unhealthy in men.
In men, the two organs responsible for Testosterone and Estrogen production are the adrenal glands and the testes. In females, the adrenal glands, as well as the ovaries, create Estrogen and Testosterone. In males, Testosterone is produced primarily, and Estrogen is produced more as a byproduct. In females, estrogen is the primary hormone produced.
The Roles of Estrogen and Testosterone in Remodeling
The sex hormones of both sexes have been linked to the production of osteoblastic cells, which work to maintain healthy bone structure. The male and female sex hormones both play their roles in maintaining homeostasis.
Progesterone and Estrogen slow down osteoclast cells, reducing the rate at which bone turnover occurs. Testosterone directly leads to the reproduction of Osteoblasts, increasing the rate at which Bone Remodeling occurs. Estrogen Deficiency causes Osteoporosis because it encourages the heightened activity of osteoclasts.
Testosterone Deficiency causes osteoporosis because it inhibits the function and production of Osteoblasts. For this reason, Testosterone and Estrogen Deficiency leads to Osteoporosis and Osteopenia. Estrogen Deficiency is uncommon in males because the body converts Testosterone into Estrogen.
The primary problem in males is that high levels of adipose fat or cortisol can upset the Sex Hormone Balance, leading to Testosterone Deficiency at the expense of Estrogen and Cortisol conversion.
Female Obesity and Osteoporosis
In females, obesity is not linked to Osteoporosis, and higher body fat levels are associated with stronger bones. Being underweight is correlated with higher rates of Osteoporosis. A healthy weight for women is enough body fat to reduce the risk of Osteoporosis, but not so much that it inhibits longevity in other ways. In males, on the other hand, obesity has been causally linked to Osteoporosis.
Healthy Testosterone Levels Encourage Male Osteoblast Production
Male muscle mass has also been shown to be linked to bone health as well. Healthy Male Testosterone Levels are vital for bone health because they encourage the activity of the osteoblasts. Although obesity leads to more outstanding Estrogen production, which slows down osteoclast metabolism, lower Testosterone levels greatly slow osteoblasts' reproduction and development, which keeps Bone Turnover Rates out of balance.
Human Growth Hormone and Bone Mineral Density Human Growth Hormone is an essential ingredient to bone health in addition to Testosterone, Estrogen, and Progesterone. Our knowledge of how sex hormones relate to Bone Mineral Density is much more evolved than our knowledge of how Human Growth Hormone contributes to bone health, but there is a direct correlation.
 Effects of HGH Deficiency Wuster's study is one of many that attempt to answer the question regarding the mechanism by which Human Growth Hormone induces bone health. The anabolic processes of Human Growth Hormone and IGF-1 cause an increase in height and bone mass during puberty.
Effects of HGH Deficiency Wuster's study is one of many that attempt to answer the question regarding the mechanism by which Human Growth Hormone induces bone health. The anabolic processes of Human Growth Hormone and IGF-1 cause an increase in height and bone mass during puberty.
Its also been shown that Healthy Human Growth Hormone levels maintain the skeletal foundation during adulthood. Adult-Onset Human Growth Hormone and IGF-1 Deficiency have also been linked to a number of adverse health outcomes regarding the aging process as well, including:
Reduced Muscle Strength and Mass IGF-1 create an energy pipeline from Adipose Fat tissue to the muscles, providing them with the energy needed to function optimally. Without proper sustenance, the muscles do not have the nutrients they need to become larger and more robust and can atrophy.
Lower Thresholds for Endurance Lower levels of energy as a result of HGH Deficiency reduce the amount of physical and mental energy at the disposal of an individual, leading to problems with cognition, focus, and physical endurance for exercise.
Increase in Adipose Fat As a result of Human Growth Hormone Deficiency, fat around the midsection begins to pool at an increased rate because IGF-1 is one of the primary metabolites which prevent fat accumulation.
Lower Bone Mineral Density IGF-1 and Human Growth Hormone encourage the production and efficiency of osteoblasts, which increase the rate at which new bone is generated, and old bone tissue is replaced.
HGH, IGF-1, and Bone Health Human Growth Hormone and its derivative IGF-1 play a direct role in overall bone health. HGH directly causes osteoblastic cells to be formed in addition to Testosterone. Although HGH is required to influence osteoblast creation, IGF-1 is necessary to encourage many of the internal processes of the osteoblast cell.
Rapid height increases during puberty primarily result from Human Growth Hormone because excess HGH bone levels encourage them to grow in length.
After the epiphyseal plates harden in late adolescence, growth no longer occurs. HGH production decreases to normal adult levels, stimulating the production of IGF-1 while not inundating the bones with excess HGH. Excess HGH levels are associated with a number of negative bone issues, such as arthritis, carpal tunnel syndrome, and acromegaly.
Acromegaly is a bone disorder in which the bones of the face, hands, and feet continue to grow past puberty due to HGH stimulation, leading to physical contortions in bone structure.
IGF-1 also affects the production of osteoblasts, but at a much more modest rate, that benefits those in adulthood. In addition, the hormone increases the functional ability of osteoblasts after creation. IGF-1 plays an integral part in average bone density and mineralization because IGF- increases the creation of collagen while inhibiting its breakdown.
IGF-1 affects the function of osteoclasts, but so far, research has been unable to precisely figure out how IGF-1 receptors on osteoclasts affect the function of those cells.
Risk Factors for Osteoporosis: Could I get Osteoporosis?
Although Osteoporosis is a fairly common disorder, it certainly does not affect all people, and one can significantly reduce the risk of the disorder through healthy living and being proactive.
There are a number of factors that can increase your chances of coming down with the disease. Some of the factors that can lead to Osteoporosis are hereditary, which results from your personal and individual genetic history. Other factors are the result of particular lifestyle and nutrition choices or the result of particular medicines.
Medical and Biological Risk Factors for Osteoporosis
Sex Females have much greater odds of being diagnosed with Osteoporosis than males. Females are 6 times more likely to be diagnosed with Primary Type One Osteoporosis and twice as likely to come down with Type Two Osteoporosis. With Secondary Osteoporosis, the odds fluctuate dependent on the root cause of Osteoporosis. There are four main reasons why women suffer from Osteoporosis more than men.
Women are, on average thinner than males. Women have naturally lighter bones than males. Menopause is correlated with a much sharper reduction in Hormone levels than male Andropause, which is a slow and steady decline that takes decades. The fourth reason is that women tend to live longer than males, and Osteoporosis is correlated tightly with age.
Race Asians and Caucasians are more likely to suffer from Osteoporosis than other races. African American women have more robust bones on average than their Caucasian counterparts. African American women experience hip breaks and fractures around half as often as their Caucasian counterparts.
Age Age is one of the most significant factors correlated with osteoporosis. Bones begin to weaken slowly, starting around the age of thirty. It takes decades for the effects of Osteoporosis to begin to show. In females, Primary Type One Osteoporosis tends to become symptomatic when women are in their fifties and sixties. Primary Type Two Osteoporosis usually occurs in the seventies or eighties. The age at which Secondary Osteoporosis occurs can vary greatly depending upon the source of bone deficiency.
Heredity Osteoporosis is highly correlated with genetic history. If older men or women in your family suffer from a spinal column or hip fracture, you may be at a greatly enhanced risk of the disorder. If you have many relatives who suffer from back issues that result in curvature of the spine and an inability to straighten the back, you are also possibly at risk.
Body Frame Women who are thin or petite are at a greater risk of Osteoporosis. Healthy body fat levels are related to elevated female Estrogen levels, which encourage the proper maintenance of bone mineral density. Women who struggle with anorexia are highly at risk for Osteoporosis, and long-term anorexia can lead to Early-Onset Osteoporosis.
Post-Menopausal Women Women who have already experienced menopause are at the highest risk of Osteoporosis because of the sharp decrease in Estrogen and other sex hormones. It takes ten to fifteen years for the symptoms to start to appear, and many women choose to undergo Estrogen Replacement Therapy to maintain the health of the bones. The bones are incredibly resilient, so it takes years of hormone deficiency for the bones to deteriorate as a result, but the deterioration is linked with high rates of mortality.
Estrogen Deficiency Females who have suffered from Estrogen Deficiency their entire lives are at a very high risk of Osteoporosis if they have not been adequately treated with Estrogen Hormone Replacement Therapy. Estrogen Deficiency can be the result of early menopause, late puberty, anorexia, or any method of suppressing the feminine cycle, as well as the total absence of sexual development.
Medicine Use A number of medicines raise the incidence of Osteoporosis because they harm bone mineralization and mass over long-term usage. Anticoagulants, Immunosuppressants, anti-epileptic drugs, and steroids have raised the risk of osteoporosis and thyroid suppression. Thyroid and Parathyroid hormones are the most direct contributors to bone health, and calcium cannot be effectively used and recycled for Bone Remodeling if these hormones are imbalanced.
Diet and Nutrition Problems Malnutrition, anorexia, chronic liver disease, and syndromes that affect the absorption of Calcium and Phosphorus can significantly increase the chances of osteoporosis.
Metabolic and Endocrine Causes Hemochromatosis, diabetes, and thalassemia increase osteoporosis risk. Thalassemia is a genetic disorder that dramatically leads to anemia and hinders bone health. Diabetes leads to erratic and abnormally high levels of blood sugar, which decrease the effect and secretion of HGH and IGF-1. IGF-1 and Human Growth Hormone are incredibly important in maintaining healthy bones, and Osteoporosis commonly results from diabetes.
Hemochromatosis is a disease that causes the body to absorb an abnormally high iron level. Although the effects of this disorder do not cause problems immediately, after thirty to forty years, the symptoms appear, and the effects can be dramatic. Excess blood-iron levels are believed to suppress osteoblast activity, leading to bone mineral breakdown and Osteoporosis over time.
Other Disorders Rheumatologic disorders, renal tubular acidosis, and certain cancers, including myeloma, mastocytosis, and Down syndrome, also increase the incidence of Osteoporosis.
Lifestyle Choices Increase Risk for Osteoporosis
Calcium Deficiency Women under fifty should consume 1000 milligrams of calcium daily. Women over seventy should have 1200 milligrams of calcium. Calcium becomes a more significant concern for males aged seventy and older
. Men under seventy should include 1000 milligrams of calcium in their diet daily. Men over that age should take or consume 1200 milligrams each day. Calcium Deficiency is defined as a daily intake of 300 mg, but recommended calcium intake is much higher.
Vitamin D Deficiency Both sexes should consume 400-800 IU of Vitamin D each day if they are less than fifty years of age. Men and women over 50 should consume 800-1000 IU. This number can vary greatly; some people need more than others. The upper safe limit for Vitamin D consumption is recommended to be 4,000 daily IU.
Caucasians and those with lighter skin are more at risk for Vitamin D deficiency. They need more daily Vitamin D. Melatonin naturally converts sunlight into Vitamin D, so African Americans and other dark-skinned people need less supplemental Vitamin D. Vitamin D is a critical component of Calcium intake which helps absorb calcium from its dietary form to a usable form. Vitamin D can be found in a number of foods, including certain fish, fortified cereals, milk, and egg yolks.
Excess Caffeine Ingestion Although it does not appear that drinking caffeine hurts calcium levels in healthy patients, those who do not consume enough calcium in their diet will find that their Calcium Deficiency is made worse by having too much caffeine.
Sedentary Lifestyle Healthy levels of Human Growth Hormone and IGF-1 are essential for maintaining healthy bones. A sedentary lifestyle is one of the worst culprits in inducing or exacerbating Human Growth Hormone Deficiency. HGH is released at its highest rates during two periods of deep sleep and exercise.
Living a life without exercise and physical exertion can lead to Hypopituitarism which inhibits the development and propagation of healthy and optimally functioning osteoblasts. In addition, the bones need exercise as much as any other organ, and physical exercise also creates pressure on the bones, encouraging the body to maintain its structural integrity.
Use of Nicotine and Tobacco Smokers lose bone density at a rate higher than nonsmokers. An analysis of twenty-nine studies shows that the risk of hip fracture increases by 17% at age sixty, 71% at age eighty, and 108% at age ninety. Although these effects are cumulative over time, deciding to quit smoking at any age will reduce the future risk of fractures associated with Osteoporosis and tobacco use.
Alcohol Heavy use of alcohol can hurt calcium absorption. Alcohol, when used in excess, can cause the pancreas to take in nutritional Vitamin D and calcium at a reduced rate. It also overloads the liver, which can reduce the efficiency of Vitamin D activation. Heavy alcohol use has been shown to destroy osteoblasts as well.
Excess alcohol can also disturb Estrogen secretion in females. Chronic alcoholism causes an increase in parathyroid hormone production as well as cortisol production. Both of these hormones harm the Bone Remodeling cycle, leaching Calcium from the bones and out through bodily excretions.
How Can I Stop Osteoporosis?
Even if you are not at a genetically high risk of Osteoporosis, there are a number of ways that you can strengthen your bones and reduce the threat of Osteoporosis.
Increase Calcium Consumption
The simplest way to reduce the risk of Osteoporosis is to take in a healthy amount of calcium daily. Choose foods that are ripe with calcium or take a daily calcium supplement in addition to the calcium you naturally take through your diet. Maintaining healthy calcium consumption throughout your life is essential because of the long-term consequences of calcium deficiency.
Poor nutrition habits you have now may come back to bite you decades later if you do not keep a preventative mindset. The bones begin to lose mass after the age of thirty, so it is essential to maintain adequate calcium levels throughout childhood and early adulthood so that your bones can be as strong as possible when decline inevitably begins.
After thirty-two, calcium intake will help minimize bone loss while strengthening bones through proper mineralization, reducing the risk of fractures later in adulthood.
If you are utilizing calcium pills, make sure that they also have Vitamin D because of the positive effect that Vitamin D has on calcium absorption. Also, pay attention to the type of calcium supplement that you buy. Calcium carbonate is inferior to calcium citrate because it is not absorbed by the body as easily. One other advantage to calcium citrate is that it does not have to be taken with food. If you use calcium carbonate, take the supplement with food to ensure sufficient absorption.
Vitamin D. Maximize Vitamin D consumption either through Supplementation or changes in diet. Although less may provide you the benefits you need, consuming 1200-2000 IU daily will ensure you get the level of Vitamin D you need at any age without putting you at any risk for too much. Again, good foods to eat for Vitamin D are Fortified foods, egg yolks, shrimp, and many fish, including pink salmon, sardines, mackerel, and halibut. Cod liver oil makes an excellent supplemental form of Vitamin D as well.
Exercise. There are three essential forms of exercise to prevent or slow down Osteoporosis. The first form of exercise is weight-bearing exercise. This exercise is simply staying on your feet and getting out and about. You can go hiking. You can dance. Anything that keeps you moving and on your feet for an extended period qualifies.
One crucial note is that biking and swimming are ineffective forms of weight-bearing exercise. Although they tax the cardiovascular system, they do not put the form of load-bearing stress on the body, which maximally benefits those at risk of Osteoporosis. Thirty minutes to an hour of physical exertion weekly is optimal to provide the best health benefits.
Resistance training is also essential when preventing or slowing Osteoporosis as well. Resistance training is simply described as weight lifting. This exercise makes the muscles more prominent and robust and helps the bones become more structurally sound.
You can lift weights or utilize spring or tube systems to provide resistance without lifting weights. Exercising in water is also very practical resistance training, especially for older men and women at high risk of osteoporosis and bone fractures.
For optimal results, one should work out in this manner at least three times each week. It is also imperative to alternate muscles to reduce wear and tear because the muscles repair and rebuild themselves primarily during rest periods.
Resistance training is practical mainly because it encourages your body to secrete more Human Growth Hormone. HGH helps make your bones more resilient and strengthens the muscles as well. For patients taking Human Growth Hormone Replacement Therapy or IGF-1 Injections, Weight training increases the effectiveness of these hormone shots.
Stretching and flexibility exercises are incredibly beneficial for those at risk for Osteoporosis. Flex exercises increase the ability of the joints to withstand stress which can significantly reduce the threat of falls or other types of injuries.
Limber joints prevent nasty falls and minor and  major bone fractures. If you are looking for a simple way to increase flexibility, going through routine stretches daily is a simple and incredibly safe way to get limber.
major bone fractures. If you are looking for a simple way to increase flexibility, going through routine stretches daily is a simple and incredibly safe way to get limber.
If you enjoy flexibility exercises and want to combine stretching with cardiovascular exercise, yoga is a fantastic way to keep in shape. If you have already had issues with Osteoporosis in the past, make sure that you engage in stretching exercises or other forms of exercise which do not overtask the hips and spinal column to reduce the risk of further issues.
The important thing is to make sure whatever you do is safe for your body. Talk to your doctor before you alter your routine of physical activity, especially if you are older and at high risk for complications resulting from Osteoporosis. It's vitally important that you engage in exercise that your body can handle while also ensuring that you are putting stress on your muscle, bones, and joints.
What Medicines Treat Osteoporosis?
As of today, there are a handful of medicines that are very effective in preventing or treating Osteoporosis.
Estrogen Hormone Replacement Therapy (HRT) Estrogen HRT has been proven to be highly effective in both staving off and alleviating the effects of Osteoporosis in women. Estrogen Treatments have been shown to decrease bone loss significantly while also boosting bone density in the hips and spine, the two areas most susceptible to Osteoporosis. The spinal column and hips are where osteoporosis creates the most devastating injuries. For female patients, the risk of bone fracture in these two vital areas is reduced significantly through Estrogen Replacement Therapy.
Estrogen Patches, Pills, and Injections Generally, Estrogen HRT is provided via patch and pill, although Estrogen injections are often used. Estrogen Injections are primarily used to alleviate the effects of menopause, and Estrogen Patches and pills are more often used to treat symptoms of low Estrogen levels such as Osteopenia, Osteoporosis, and low libido.
Estrogen Hormone Treatments are effective when begun at any age, but they are most effective when used as a preventative measure to attempt to bypass Osteoporosis altogether.
Estrogen Replacement Therapy is Paired with the Hormone Progestin One of the main risks associated with taking Estrogen Replacement Therapy alone is that it can raise the risk of experiencing endometrial cancer, which is a cancer of the uterine lining. In the menstrual process, spikes in estrogen levels cause the line of the uterus to thicken in a monthly cycle. Excess use of Estrogen can lead to undesired growth of endometrial tissue, which can, in some cases, develop into cancer.
New therapies have been created that significantly reduce the risk of endometrial cancer when utilizing Estrogen Hormone Replacement Therapy. In most cases where Estrogen HRT is utilized, a hormone known as progestin is provided alongside estrogen in patients who still have a uterus.
Progestin prevents endometrial hyperplasia, the rapid build-up of endometrial cells resulting from unopposed Estrogen Replacement Therapy.
Why are Estrogen and Progestin used together? Generally, in a hormonally stable woman, Estrogen and Progestin work as counterbalances to one another to maintain the normal cycle of endometrial development. After menopause, the release of both of these hormones drops precipitously.
Because introducing exogenous Estrogen does not cause an increase in progestin, progestin must be supplementally supplied as well.
Side Effects of Estrogen HRT Side effects of Estrogen Hormone Replacement Therapy include hypertension, breast sensitivity, bloating, and nausea. Evidence suggests that high blood pressure can be an issue in female patients utilizing birth control products, including estrogen. Estrogen Replacement Therapy provides a much lower level of Estrogen, which is not believed to lead to hypertension.
Water Retention is a direct result of estrogen use and, in most patients, will not be an issue or will not be severe enough to suspend or alter therapy. Suppose you experience bloating as a result of Estrogen Replacement Therapy. In that case, you can talk to your doctor about dietary changes to resolve bloating issues, and there are also medications you can take that will help to resolve the issue.
Some patients respond to oral estrogen negatively and experience nausea as a result. For these patients, switching to a patch should resolve the issue entirely. Breast tenderness can be resolved by changing to a patch or adjusting the dosage.
Estrogen and Breast Cancer Risk
The current body of scientific evidence does show that long-term Estrogen Replacement Therapy is correlated with an increased risk of breast cancer, so if you are at an increased risk of breast cancer or currently have breast cancer, you should avoid Estrogen HRT unless you have been given the okay by  your physician.
your physician.
Although Estrogen Replacement Treatments are effective at alleviating Osteoporosis, it is not commonly prescribed for periods more extended than a few years because of the increased risk of breast cancer that occurs with prolonged usage.
Testosterone Hormone Replacement Therapy
Testosterone HRT is often effective in male patients who suffer from Osteoporosis. Male Osteoporosis often goes unidentified and misdiagnosed because of its relative rarity. Still, male hypogonadism can lead to a hormone imbalance which can negatively impact the bone mineral density of the skeletal system.
Male Osteoporosis Less Common
Although Male Osteoporosis is much less common, it is still a significant issue that occurs with enough frequency that male bone health should be cautiously monitored with age. Testosterone plays a vital role in the maintenance and proliferation of osteoblasts. Patients who suffer from Low Testosterone, especially those with total hypogonadism, need Testosterone Treatments to strengthen the bones and maintain physical strength, cognitive ability, and sexual libido.
Increase in Male Osteoporosis in Recent Years
There has been an uptick in diagnoses of Male Osteoporosis in the last generation, and several factors may contribute to this. Men live longer than they once did and are more prone to experiencing Primary Type Two Osteoporosis, which tends to affect males in their seventies and eighties rather than earlier in life, like Primary Type One Osteoporosis, which affects females significantly more than males.
Osteoporosis and the Sedentary Workplace
Also, because males are more often working in sedentary environments, Testosterone Deficiency is more of an issue than ever before. In Great Britain, for example, it is believed that Osteoporosis affects one in every twelve men, and one in every six males over the age of eighty will experience a fractured hip at some point in the rest of their life. In scientific research, men who suffer from hypogonadism have been shown to experience rates of bone turnover that are far higher than healthy men.
Male patients who have experienced minor hip or spinal fractures are encouraged to seek Testosterone Replacement Therapy. In addition, Hypo-gonadal patients who have been proven to have reduced Bone Mineral Density will also likely benefit significantly from Testosterone injections.
Testosterone Replacement is a Natural Therapy
Many physicians are now recommending Bio-Identical Testosterone HRT as an alternative to Bisphosphonates because Testosterone HRT is a much more natural form of therapy that mimics and enhances the body's natural processes. With all of the other positive benefits of Testosterone Replacement Therapy for Osteoporosis, it seems to be a clear choice for male patients as Osteoporosis and Low-T manifest themselves with age.
Testosterone Replacement Therapy for Low-T and Osteoporosis produces minor or no side effects in most patients. The most reported side-effects of BioIdentical Testosterone Hormone Replacement are skin abrasion and rashes at the administration site, slightly increased hemoglobin count, decreased HDL (Healthy Cholesterol), and acne.
Testosterone Replacement Therapy Produces Few Significant Side-Effects
A cross-section of ten studies showed no significant adverse reaction to therapy in any trials. Testosterone should not be used by patients suffering from prostate cancer because Testosterone Hormone Replacement Injections can exacerbate existing prostate tumors. Also, patients who utilize anti-coagulants should be especially cautious with Testosterone Replacement because of the effect that Testosterone Replacement sometimes has on hemoglobin counts.
Human Growth Hormone Replacement Therapy
Growth Hormone Injections are a new method for Osteoporosis treatment compared to the others listed, but it still shows promising results. The Wuster Study cited earlier in this article is evidence in favor of Human Growth Hormone HRT, and many other studies present similar evidence. HGH Hormone Replacement Therapy works by encouraging the proper function of Osteoblasts through the intervention of exogenous IGF-1.
HGH Makes Osteoporosis Prevention Easier
In addition, HGH Hormone Treatments also encourage physiological changes, which lead to enhanced outcomes. Human Growth Hormone alleviates adipose fat accumulation, discouraging excess estrogen production in males and increasing the effectiveness of endogenous HGH secretions.
HGH Injections also have a tendency to reduce fatigue and bolster muscle mass and strength, which helps patients maintain an exercise program that can help them strengthen their bones and muscles in a way that enhances outcomes and reduces the risk of fractures in the future in patients who suffer from either osteopenia or osteoporosis.
HGH Treatments Have Low Incidence of Major Side-Effects
Only minor side effects were reported in studies regarding HGH Hormone Replacement Therapy for the Treatment of Male Osteoporosis. The vast majority of patients did not suspend treatment due to the therapy.
For female patients, there is a high likelihood that HGH Hormone Replacement Therapy will cause Estrogen Replacement for Osteoporosis to fall out of favor. For men, on the other hand, it appears that a combination of HGH and Testosterone HRT may produce the best outcomes regarding both Osteoporosis and overall life quality.
Bisphosphonates
Bisphosphonates are medications that can slow down the rate at which bones are broken down by osteoclasts, inhibiting the resorption of bone tissue. By slowing down the effect of resorption, Bisphosphonates can stabilize the Bone Remodeling process to increase the bones' structural strength, decreasing the dangers of Osteoporosis. These medicines have been proven to boost bone mineral density while lowering the incidence of spinal cord and hip fractures.
The Food and Drug Administration-approved Bisphosphonate medication for post-menopausal females is known as Alendronate. Bisphosphonates produce a few side effects, the most constant being gastrointestinal discomfort and acid reflux. These issues can be resolved by taking the medication without food or an entire glass of water. Also, remain sitting or standing for a half-hour after taking the medication to prevent stomach discomfort.
Atrial Fibrillation and Bisphosphonates
Another more dangerous side effect that is believed to result from the usage of Bisphosphonates is atrial fibrillation. Around one in every thirty cases of atrial fibrillation results from using Bisphosphonates. Female patients at risk for cardiovascular disease, heart attacks, or diabetes should only use this drug at their physician's recommendation while considering cost-benefit analysis.
Bisphosphonates and Femur Fractures
In sporadic cases, femoral fractures can result from Bisphosphonate Therapy, but this occurs in fewer than 1 per 1000 cases, and the benefits exceedingly outweigh the risk of this issue. This is believed to occur because long-term suppression of Bone Remodeling prevents the 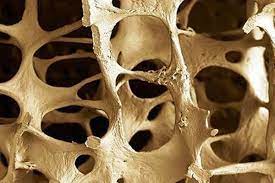 femur from recovering from minor structural issues.
femur from recovering from minor structural issues.
This drug can break down osteoclasts, and as a result, the bone is not broken down for recycling by osteoclasts, and bone structural integrity very slowly declines. Over time in this minority of cases, microfractures combine into large and more fragile areas prone to more significant fracture.
Calcitonin
This form of therapy is a potential advantage for females who cannot utilize Estrogen HRT or other forms of Hormone Replacement. Calcitonin can be prescribed for female patients that passed through menopause a minimum of five years before the prescription. For these women, Calcitonin can be used to raise the density of the spinal column while reducing bone mass atrophy.
Calcitonin (also known as thyrocalcitonin) is a thyroid hormone that promotes stronger bones by helping maintain healthy phosphorus and calcium metabolism.
Because Calcitonin is a complex hormonal protein, it cannot be taken orally. The liver would break down the hormone before it had the opportunity to function because of its structure.
Calcitonin can be delivered either as a nasal spray absorbed into the sinus membrane or as a Calcitonin Shot. Calcitonin inhibits the function of Osteoclasts, reducing the rate at which Bone Resorption takes place while also having a beneficial effect on cartilage formation.
Selective Estrogen-Receptor Modulators
These medicines and molecules can emulate the function of Estrogen on certain Estrogen Receptors. Depending on their structure, different SERM medications can mimic different aspects of Hormonal Estrogen. Three common forms of SERM used for the treatment of Osteoporosis are Femarelle, Lasofoxifene, and Raloxifene.
These drugs can also resolve other issues, including but not limited to Menopause Management, Breast Cancer, and Contraception.
Raloxifene Best SERM for Osteoporosis
Raloxifene is particularly effective at resolving Osteopenia and Osteoporosis issues in the spinal column and the hips. For this reason, the drug has been FDA-approved as the most effective SERM for bone health and osteoporosis prevention.
Although the drug does benefit the skeletal system, current evidence shows that Raloxifene is less effective at alleviating and preventing spinal osteoporosis than either Calcitonin, Estrogen Replacement Therapy (for women), or Testosterone Replacement Therapy (for men).
One of the most significant benefits of this drug is that side effects are infrequent, so the drug can be incredibly beneficial for patients who cannot utilize Hormone Replacement Therapy or Calcitonin treatment.
A tiny minority of female patients have reported hot flashes similar to those experienced during menopause. An even smaller subset reported Deep Vein Thrombosis, a potentially dangerous blood clot in the leg.
Conclusion: Osteoporosis and Hormone Replacement Therapy
A number of remedies can be used to prevent or alleviate the symptoms of Osteoporosis. Although many different options provide their benefits and potential drawbacks, Hormone Replacement Therapy is often the most effective form of treatment.
Benefits of Estrogen Replacement Therapy
Estrogen Replacement Therapy can be very beneficial for short to intermediate-term treatment of Female Osteoporosis. In addition to this, Estrogen HRT has also been shown to provide these other benefits as well:
- Alleviating the effects of Menopause, reducing the severity of hot sweats and cold flashes
- Improves mood stability after menopause
- Decreases incidence of insomnia and sleeping disorders in post-menopausal patients
- Produces healthier skin by increasing collagen levels in the outer layers, smoothing wrinkles, and tightening the muscles of the face
- Alleviates the symptoms of Peri-menopause and Early-Onset Menopause
- Increases libido and alleviates vaginal dryness during menopause
Because long-term use of Estrogen can increase the risk of breast cancer, long-term use of Estrogen Replacement Therapy is not usually recommended. Still, Estrogen Replacement Therapy utilized in menopause can delay the symptoms of Osteoporosis by preserving bone health.
The risks in utilizing Estrogen HRT are very low when used for a relatively short time, but utilizing the treatment for ten or more years may lead to unacceptable breast cancer risk. In the future, these recommendations may change significantly because newer research suggests that Estrogen Replacement Therapy can effectively maintain bone health even at very low doses, which do not significantly increase the risk of breast cancer.
Benefits of Testosterone Replacement Therapy
Testosterone HRT is one of the most talked-about Hormone Treatments available in the United States today. Although the body of research is not as large as that for Estrogen Hormone Replacement, there is significant evidence that Testosterone HRT can be highly beneficial for male patients at risk of experiencing Osteoporosis or Low Bone Density.
Hormone Replacement Therapy with Testosterone produces a number of other benefits which can make Osteoporosis prevention seem like an added bonus. The following are expected benefits of Testosterone Replacement Treatments:
- Increases in libido
- Resolves sexual dysfunction and alleviates premature ejaculation
- Boosts and/or preserves muscle mass
- Enhances cognition and memory faculties
- Prevents depression and stabilizes mood while suppressing anxiety
- Alleviates pain in the joints and muscles
- Increases energy and reduces feelings of exhaustion
- Raises one's overall sense of well-being
Some side effects are associated with Testosterone Injections, patches, and creams. Still, significant side effects are infrequent for patients who utilize low-dose Testosterone treatments for Testosterone Deficiency.
The vast majority of patients either experience no side effects or minor side effects. It is estimated that Testosterone Replacement Therapy for Low-T can actively benefit half of the men in their fifties. The number is even higher for men in their sixties: sixty percent!
As the body of knowledge surrounding Testosterone as an Anti-Aging Therapy grows, new and perhaps more incredible benefits will be revealed.
Benefits of Human Growth Hormone Replacement Therapy
HGH Hormone Replacement Therapy has only been studied as a potential treatment for Osteoporosis in recent years, but the benefits seem to show  high levels of potential. HGH proves time and time again that it is a vital hormone that significantly alleviates the negative aspects of the aging process while preserving optimal function and metabolism in multiple systems of the body.
high levels of potential. HGH proves time and time again that it is a vital hormone that significantly alleviates the negative aspects of the aging process while preserving optimal function and metabolism in multiple systems of the body.
We may eventually find that HGH plays at least some role in every necessary body process.
Dr. Wusters's recent Human Growth Hormone for Osteoporosis study shows that HGH can increase bone density due to the positive interaction between HGH, IGF-1, and the osteoblast. This form of therapy seems equally beneficial for both men and women.
This treatment is also likely safer and provides similar benefits to Estrogen Replacement Therapy for Osteoporosis without producing increased cancer risk side effects.
HGH Shots also provide a number of other significant benefits in addition to the prevention of Osteoporosis, including, but not limited to:
- Increased metabolism
- Breakdown of unhealthy adipose fat tissue
- Increase in muscle mass and strength
- Improved sleeping habits
- Boosted nutrient absorption
- Enhanced Energy
- Reduced Fatigue
- Increase overall sense of well-being
Although there is a particular risk for side effects when using Human Growth Hormone, these risks are generally associated with individuals who abuse the drug for performance enhancement. HGH is not legal for use as a PED in the United States and can only be used by those with a diagnosable Human Growth Hormone Deficiency or other legitimate medical conditions such as Hypopituitarism or Childhood Idiopathic Short Stature.
The Conscious Evolution Institute
The Conscious Evolution Institute is one of the nations leading Anti-Aging and Regenerative clinics. Osteoporosis is one of the most devastating conditions related to the aging process. Sadly, if more men and women were proactive, the disorder would be much less prominent than it is today. There are many ways to treat the disease, and for many individuals, Hormone Replacement Therapy with Testosterone, Estrogen, or HGH may be the correct answer.
We urge you to give us a call today if you are feeling the effects of Hormone Deficiency. There is no pressure to commit, and we have a friendly, knowledgeable, and experienced staff that will be happy to take the time to answer any questions you may have about our treatment options.
At the Conscious Evolution Institute, we work with you to create a life plan to help you maximize Hormone Replacement's benefits. It's not just a medical treatment; it's a lifestyle revolution.
In addition to your Hormone Medications, we will also work with you to design a workout and nutrition plan to help you get into shape. We have helped thousands of men and women across the United States alleviate and reverse the effects of aging, and we want to help you as well.
National Network of Conscious Evolution Institute Affiliates
If you are interested in the treatments we provide, please fill out the form on our website or call our toll-free number today. We have a certified network of  affiliated physicians across the United States, so you do not need to visit us in person. Our affiliates gather all the necessary data we need to provide an accurate diagnosis, including Family History, Blood Samples, and Routine Physical.
affiliated physicians across the United States, so you do not need to visit us in person. Our affiliates gather all the necessary data we need to provide an accurate diagnosis, including Family History, Blood Samples, and Routine Physical.
After we receive your diagnostic data, we will have everything we need to make an accurate diagnosis. You will receive your diagnosis in around five business days! After we fill out your prescription, we can ship the product via FedEx straight to your door. It's just that easy. Again, we encourage you to call us today at the Conscious Evolution Clinic.
Don't put it off any longer. If you are over thirty and feel the aging process's adverse effects, we can help! We look forward to hearing from you.
Yours in Longevity,
The Conscious Evolution Institute
- 0001) Regular Physical Activity Will Boost Your Mood and Reduce Stress [Last Updated On: February 13th, 2025] [Originally Added On: December 31st, 2020]
- 0002) Ten Natural Ways To Reduce Anxiety [Last Updated On: November 19th, 2025] [Originally Added On: January 1st, 2021]
- 0003) Nbc News: Men's Magic Youth [Last Updated On: April 13th, 2025] [Originally Added On: January 2nd, 2021]
- 0004) My Own Experience With Human Growth Hormone (case Study) [Last Updated On: November 18th, 2025] [Originally Added On: January 3rd, 2021]
- 0005) Treating Polio Virus and Post Polio Syndrome With Human Growth Hormone Injections [Last Updated On: November 28th, 2025] [Originally Added On: January 4th, 2021]
- 0006) Outline Of The Benefits Of Human Growth Hormone [Last Updated On: November 17th, 2025] [Originally Added On: January 6th, 2021]
- 0007) Eight Tricks To Relieve Inflammation [Last Updated On: February 19th, 2025] [Originally Added On: January 7th, 2021]
- 0008) Tips and Tricks on How to Naturally Lower Your Blood Pressure [Last Updated On: December 7th, 2025] [Originally Added On: January 8th, 2021]
- 0009) When Is the Best Time to Start HGH Treatment? [Last Updated On: October 20th, 2025] [Originally Added On: October 11th, 2021]
- 0010) How Fast Can I Get Results With HGH Therapy? [Last Updated On: April 15th, 2025] [Originally Added On: October 23rd, 2021]
- 0011) New Brain Receptor Found that Could Help Keep Our Minds Healthier Longer [Last Updated On: February 14th, 2025] [Originally Added On: May 17th, 2022]
- 0012) A Medical Doctor Tries Human Growth Hormone In 1992 [Last Updated On: February 14th, 2025] [Originally Added On: May 19th, 2022]
- 0013) How Hormones Control Hunger and Satiety [Last Updated On: February 14th, 2025] [Originally Added On: May 22nd, 2022]
- 0014) It’s Amazing! Bible Hero Noah and HGH [Last Updated On: October 21st, 2025] [Originally Added On: December 13th, 2022]
- 0015) How Can I Tell if I Have a Hormone Deficiency? [Last Updated On: February 19th, 2025] [Originally Added On: January 10th, 2023]
- 0016) Is HGH the Miracle Therapy that Countless People have Been Waiting for all Their Lives? [Last Updated On: March 7th, 2025] [Originally Added On: January 25th, 2023]
- 0017) County Lineman Gets His Life Back [Last Updated On: April 21st, 2025] [Originally Added On: February 10th, 2023]
- 0018) Abused Woman Discovers the Power of Hormone Replacement Therapy [Last Updated On: April 10th, 2025] [Originally Added On: March 1st, 2023]
- 0019) Which HGH Booster or HGH-boosting Supplement Should I Buy? [Last Updated On: April 18th, 2025] [Originally Added On: March 17th, 2023]
- 0020) Scene from an As-Yet Unreleased Documentary: “I was Suffering, and I Didn't Know I Had an HGH Deficiency” [Last Updated On: April 29th, 2025] [Originally Added On: May 17th, 2023]
- 0021) Human Growth Hormone Improves the Immune System [Last Updated On: May 2nd, 2025] [Originally Added On: June 9th, 2023]
- 0022) What Happens if You Forget a Dose? [Last Updated On: August 15th, 2025] [Originally Added On: August 23rd, 2023]
- 0023) What Scientists Successfully Synthesized Human Growth Hormone (HGH) for the First Time? [Last Updated On: September 7th, 2025] [Originally Added On: September 18th, 2023]
- 0024) Identifying Hormonal Deficiency: Common Symptoms [Last Updated On: February 19th, 2025] [Originally Added On: February 11th, 2025]
- 0025) The Potential of HGH as a Life-Changing Therapy [Last Updated On: March 3rd, 2025] [Originally Added On: March 3rd, 2025]
Word Count: 9784






