Low Testosterone Affects A Third Of Young Men With Type 2 Diabetes
Video Link: https://vimeo.com/187730095
Video Download: Low Testosterone Affects A Third Of Young Men With Type 2 Diabetes
Video Stream: Low Testosterone Affects A Third Of Young Men With Type 2 Diabetes

One-Third of Type-Two Diabetics Suffer from Testosterone Deficiency
A new study shows that young male patients with Type-Two Diabetes have a significantly high risk of developing Testosterone Deficiency at an early age. This study shows that around one in three patients between 18 and 35 suffer from Clinically Low Levels of Testosterone.
Diabetes-Testosterone Study Information
The primary investigator in this study was Dr. Paresh Dandona. He and his associates performed their research at the New York State University of Buffalo. This study compared 62 diabetic patients. 24 of the men had been previously diagnosed with Type-Two Diabetes, and 28 of the participants were males with Type One Diabetes.
Blood testing revealed that patients with Type-Two Diabetes had much lower endogenous Testosterone Levels than the male patients with Type One Diabetes.
33% of the subjects with Type-Two Diabetes were found to have clinically low levels of Testosterone, and 58% of this group had Testosterone levels that were abnormally low compared to healthy patients.
Type-One Diabetes patients did not suffer from this clinical medical issue, however. Only 8% of Type-One Diabetics were found to have Testosterone levels that were at all abnormal.
Testosterone Deficiency Linked to FSH Deficiency and Luteinizing Hormone Deficiency
Patients in this study that were found to have low levels of Testosterone were also shown to have medically low levels of Follicle-Stimulating Hormone and Luteinizing Hormone. As a result, these patients clinically suffered from a disorder known as Hypogonadotropic Hypogonadism.
This disorder greatly enhances the risk of a number of medical disorders if left untreated, including cardiovascular disease and osteoporosis. Other symptoms of Hypogonadotrophic Hypogonadism include infertility, impotence, and lack of libido.
Type-Two Diabetics are High-Risk Patients for Low Testosterone
In the end, the researchers concluded that young patients suffering from Type-Two Diabetes are an incredibly at-risk subset of the population for suffering from Low-T, even in their twenties. Both Free Testosterone levels and Total Testosterone levels are significantly affected.
As a result of this deficiency, in combination with deficiencies in Luteinizing Hormone and Follicle-Stimulating Hormone, these patients are at a high risk of a number of cardiovascular and sexual medical conditions. They need to be treated with Testosterone Hormone Replacement Therapy to minimize health risks and help them live healthier and more fertile life.
Facts About Testosterone Deficiency
Testosterone Deficiency is a prevalent symptom of both diabetes and obesity. Around one-third of males with Type-Two Diabetes will also suffer from the symptoms of Testosterone Deficiency as a result. The clinical term for Low-T is known as Hypogonadism.
Symptoms of Low-T
There are a number of symptoms related to Low Testosterone. Among these symptoms are:
Decreased sex drive Low Testosterone reduces sexual desire in males, leading to bedroom dissatisfaction and contributing to rocky relationships
Depression Testosterone plays a significant role in male mood stabilization. Males who suffer from Hypogonadism are more likely to experience feelings of sadness and depression that they cannot shake.
Fatigue and exhaustion Testosterone is a vital component of male metabolism. Although Human Growth Hormone directly causes enhanced metabolism, Low Testosterone causes muscle strength and cardiovascular stamina problems.
Bone health deterioration Patients who suffer from Low-T are at an increased risk of bone disorders such as osteoporosis. Loss of Bone Mineral Density can even make you grow shorter over time!
Reduced strength Testosterone is directly responsible for the differences in muscle strength and muscle mass that separate males and females. Testosterone can amplify the effects of weight training and muscle building. Men who suffer from Low-Testosterone lose their ability to generate and sustain additional muscle.
Decreased erectile sensitivity Healthy Testosterone Levels are necessary for men to experience optimal pleasure in sexuality. Patients with Low-T often complain the sex just doesn't feel like it used to, which puts a damper on sex drive and libido.
Fertility Testosterone is an essential factor in the production of healthy sperm. Individuals with low levels of Testosterone have lower sperm counts than those who have healthy Testosterone levels. In addition, normal Testosterone levels are vital for healthy and fully functional sperm.
Smaller testicles One of the most apparent visible symptoms of Testosterone Deficiency is testicular shrinkage. Without sufficient levels of Testosterone, the Testicles are not as healthy or functional, and one of how this can be seen is through testicular size and shape.
Reduced sexual ability Men with Low Testosterone complain that their disorder prevents them from even engaging in satisfying sexual activity. Testosterone is a big part of what allows a man to get turned on. When Testosterone levels in the body are insufficient, the physiological process which produces a firm, hard erection is hindered.
Increased inflammation Low Testosterone is correlated with increased levels of cortisol, the human body's central agent of inflammation, which can cause pain and slow the body's natural healing processes.
Low-T Exacerbates Symptoms of Diabetes
Testosterone Deficiency has been shown to make the symptoms of diabetes worse. In addition, suffering from Low Testosterone while dealing with Diabetes can increase the risk of heart complications such as stroke, cardiovascular disease, and high cholesterol.
Dr. Paresh Dandona and Dr. Sandeep Dhindsa have dedicated their careers to the study of Diabetes. They have found a number of critical links between Type-Two Diabetes and Testosterone Deficiency.
Type-Two Diabetes Hastens Declining Testosterone Levels
Testosterone levels naturally decline over time, beginning in the late twenties, and this decline continues throughout the lifespan. In otherwise healthy individuals, this decline occurs at a rate of between one or two percent each year, similar to the rate at which Human Growth Hormone levels decline. Several medical conditions increase the rate at which Testosterone Decline occurs, and other disorders significantly reduce Testosterone Levels very quickly.
Type-Two Diabetes significantly depresses natural Testosterone levels, leading to several life-changing and potentially dangerous side effects. Studies like the one we mentioned at the beginning of this article have led endocrine scientists to conclude that four out of every ten men who suffer from obesity will have clinically low levels of Testosterone compared to males of the same age who are not overweight.
The resulting difference is even more profound when diabetes is thrown into the mix. Low-Testosterone levels plague fifty percent of obese males clinically diagnosed with diabetes.
Type-Two Diabetics Suffer Primarily from Secondary Hypogonadism
One may conclude that the primary correlation here would be between weight and testosterone level, but this is not necessarily the case. Although obese and diabetic men are most at risk of Low Testosterone Levels, there is ample evidence that Type-Two Diabetes significantly reduces Testosterone Levels even in patients who do not suffer from weight issues. This suggests that Type-Two Diabetes seriously inhibits the human body's ability to produce testosterone directly.
Type-Two Diabetes Equivalent to Twenty Pounds of Fat
Dr. Dhindsa, one of the primary investigators of the study discussed at the beginning of this article, says that Diabetes has an effect on Testosterone Levels that can be correlated with weight gain. He says that those suffering from Type-Two Diabetes experience a decline in Testosterone levels, equivalent to gaining twenty pounds of body fat.
Another study produced by Dr. Dhindsa shows that endogenous Testosterone production declines at a rapid and non-linear rate dependent upon Body Mass Index. The more an individual weighs, the more likely they will suffer from an acute deficiency of Testosterone.
Most extensive Testosterone-Diabetes Study Ever Conducted.
Dr. Dandona and Dr. Dhindsa have been responsible for the most extensive study regarding Testosterone, Diabetes, and Obesity ever conducted. Before these two doctors began their study, most research regarding Testosterone Deficiency was only concerned with patients who suffered from obesity or patients who suffered from Diabetes. These two doctors focused on how the two diseases interact and amplify the symptoms of Testosterone Deficiency.
Their most extensive study utilized data from the 2003-2004 Hypogonadism in Males study. This clinical study involved over 1800 males from 95 medical clinics. The study was underwritten by the company Solvay Pharmaceuticals.
The scientists recommend that males with diabetes and obesity keep a close eye on their Testosterone Levels. Healthy Testosterone levels are an essential part of living a healthy life, and Low-Testosterone can increase the dangers of both diabetes and obesity while also preventing patients from being able to manage their disease successfully. Dr. Dhindsa's primary goal as a medical researcher is to improve treatment options for male patients who suffer from Hypogonadism and diabetes.
Dr. Dandona is primarily interested in the effects and causes of Low Testosterone in younger men who should be participating in the most reproductive period of their lives.
Questions about Testosterone Deficiency
What is Follicle-Stimulating Hormone?
Follicle-Stimulating Hormone (often abbreviated as FSH) is a member of a group of hormones known as Gonadotrophins. Gonadotrophins are hormones responsible for stimulating the sexual organs, which are vital for healthy sexual function.
These hormones are derivatives of Testosterone and Estrogen, which promote the normal function of the testes and the ovaries. FSH is both manufactured and secreted by the pituitary.
In females, FSH increases the formation of egg follicles while also stimulating the ovulation process. In males, FSH primarily stimulates a group of cells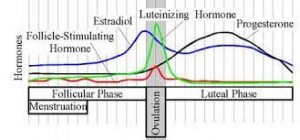 known as Sertoli cells.
known as Sertoli cells.
These cells are responsible for the healthy development of sperm cells. Low Levels of FSH in adults have no real negative consequences outside of fertility issues, but monitoring FSH levels helps doctors identify the exact source of Testosterone Deficiency.
In young boys and girls experiencing puberty, however, low levels of FSH can hinder the proper development of the testes and ovaries, significantly affecting the development of secondary sexual characteristics.
What is Luteinizing Hormone?
Although Follicle-Stimulating Hormone and Luteinizing Hormone are both Gonadotrophins, a deficiency of Luteinizing Hormone is much more harmful to human physiology. The Luteinizing hormone is sometimes referred to as Lutropin. The pituitary gland produces this hormone by formations known as Gonadotroph Cells. These cells are located in the anterior portion of the pituitary.
In women, Luteinizing Hormone is the base trigger mechanism for ovulation. In males, the hormone is responsible for stimulating the production of Testosterone by triggering the function of Leydig cells. In males, a deficiency of Luteinizing hormone can contribute to a number of adverse symptoms, including Testosterone Deficiency and the symptoms inherent with that Deficiency.
Luteinizing hormone deficiency during puberty can delay and limit natural changes. A Testosterone Deficiency combined with a deficiency of FSH and Luteinizing Hormone is known as Idiopathic Hypogonadotropic Hypogonadism.
What is Hypogonadism?
Hypogonadism is the blanket term for any disorder which prevents the human body from optimally producing sex hormones such as Testosterone, Estrogen, and Progesterone. Adult-onset Testosterone Deficiency is a form of Hypogonadism that generally results from the testes' slow and steadily decreased hormone production.
Hypogonadism as a result of Obesity and Type-Two Diabetes is the result of the conversion of existing Testosterone into Estrogen and Cortisol and reduced input from the hypothalamus and pituitary gland.
What is Hypogonadotrophic Hypogonadism?
Hypogonadotropic Hypogonadism is a form of gonadal deficiency resulting from an insufficiency of the pituitary gland or the hypothalamus. This range of disorders is also referred to as Secondary Hypogonadism.
Primary Hypogonadism is the result of a hormonal deficiency of the sex organs. Adult-onset, age-related Testosterone Deficiency is generally related to Primary Hypogonadism. Testosterone Deficiency resulting from Type-Two Diabetes is primarily the result of Secondary Hypogonadism, which is why the disorder is very powerful and not related to average testosterone decline due to aging.
There are a few essential steps to normal testicular function. The hypothalamus releases a hormone known as Gonadotropin-Releasing Hormone, 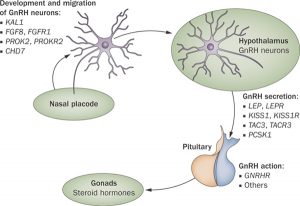 abbreviated GnRH. GnRH then flows from the hypothalamus to the anterior pituitary gland. After stimulation, the pituitary gland secretes and releases the hormones FSH and Luteinizing Hormone.
abbreviated GnRH. GnRH then flows from the hypothalamus to the anterior pituitary gland. After stimulation, the pituitary gland secretes and releases the hormones FSH and Luteinizing Hormone.
These hormones then move through the bloodstream down to the male and female sex organs, where they stimulate the average production of sex hormones such as Testosterone and Estrogen, as well as other important hormones which control sexual function.
Suppose there is a hormonal imbalance between the hypothalamus and the sex organs. In that case, this can significantly alter average hormone production, which is detrimental to human health.
Although there are some forms of extreme or total Hypogonadotrophic Hypogonadism, Diabetes and obesity produce a moderate form of Hypogonadotrophic Hypogonadism, which causes a number of detrimental symptoms which are very similar to Age-Related Testosterone Deficiency as a result of Andropause.
Most individuals will not experience the adverse effects of Testosterone Deficiency until their thirties and forties, but patients who suffer from Hypogonadotrophic Hypogonadism often experience hormonal issues from birth. Many others, as is the case with those suffering from Type-Two Diabetes, begin to experience the symptoms of Testosterone Deficiency in their early twenties.
What is the importance of these Testosterone Deficiency Studies?
Dr. Dandona's research study sheds significant light on how Testosterone Deficiency, Obesity, and Diabetes interact. The pathology of Testosterone Deficiency in Type-Two Diabetes does not seem to be related to an insufficiency of the testes but to issues resulting from hormonal balance resulting from the pituitary gland and the hypothalamus.
This causes symptoms of hormonal deficiency, which generally do not begin to occur until patients are in their thirties and forties, to appear while patients are in their twenties.
Fatigue and exhaustion prevent patients from efficiently engaging in exercise, and changes in muscular metabolism prevent them from building muscle due to exercise. Low Testosterone also encourages higher levels of cortisol and estrogen, which are detrimental to male patients and significantly reduce cardiovascular health.
Obesity complicates issues with Low Testosterone and Type-Two Diabetes by increasing the rate at which Testosterone is converted into estrogen by the fat cells. Adipose fat tissue naturally can convert Testosterone into Estrogen and Estrogen-related hormones. The more fat tissue in the body, the less impact endogenous Testosterone produces on the human body.
Scientific evidence shows that Type-Two Diabetes and Obesity are intricately connected in a number of ways, although not all diabetics are obese, and not all obese individuals develop diabetes.
Diabetes reduces the effectiveness of insulin in processing blood sugar, making it harder to maintain a healthy body weight, and deteriorates physical health in numerous ways. Dr. Dandona's study shows that both obesity and Type-Two Diabetes impact Testosterone negatively via their own unique yet interconnected pathways.
Also, the study shows that Testosterone Hormone Replacement Therapy can be a highly beneficial treatment that alleviates some of the effects of Diabetes while also improving metabolism, boosting energy levels, and encouraging weight loss to help obese patients lose weight and improve their BMI.
If you suffer from Type-Two Diabetes, we encourage you to monitor your testosterone levels closely. Although you may be in control of your insulin levels, you may be allowing Low Testosterone to decrease the quality of your life significantly. To learn more about Testosterone Hormone Replacement Therapy, contact the Conscious Evolution Institute with any questions!
- 0001 What Are Normal Testosterone Levels For Men And Women Throughout Life? [Last Updated On: February 14th, 2025] [Originally Added On: May 26th, 2020]
- 0002 Top Tips For Boosting Testosterone Naturally [Last Updated On: September 27th, 2025] [Originally Added On: May 27th, 2020]
- 0003 The Testosterone Factor [Last Updated On: October 28th, 2025] [Originally Added On: May 28th, 2020]
- 0004 Testosterone Can Help Relieve The Menopause Symptom Of Hot Flashes [Last Updated On: February 14th, 2025] [Originally Added On: May 29th, 2020]
- 0005 How Does Low Testosterone Cause Infertility? [Last Updated On: February 8th, 2025] [Originally Added On: May 30th, 2020]
- 0006 The Benefits Of Testosterone Therapy For Prostate Cancer [Last Updated On: February 14th, 2025] [Originally Added On: May 31st, 2020]
- 0007 Is Testosterone Replacement A Valid Diabetes Treatment? [Last Updated On: February 15th, 2025] [Originally Added On: June 1st, 2020]
- 0008 Testosterone Shock Therapy May Be An Effective Prostate Cancer Treatment [Last Updated On: February 5th, 2025] [Originally Added On: June 2nd, 2020]
- 0009 Testosterone Replacement Therapy Is Safe For The Heart [Last Updated On: February 14th, 2025] [Originally Added On: June 3rd, 2020]
- 0010 Testosterone Replacement Therapy [Last Updated On: October 22nd, 2025] [Originally Added On: June 4th, 2020]
- 0011 Testosterone Patches [Last Updated On: February 8th, 2025] [Originally Added On: June 5th, 2020]
- 0012 Testosterone Overview [Last Updated On: February 13th, 2025] [Originally Added On: June 6th, 2020]
- 0013 Testosterone Levels And Making Money [Last Updated On: September 10th, 2025] [Originally Added On: June 7th, 2020]
- 0014 Testosterone Enanthate [Last Updated On: September 9th, 2025] [Originally Added On: June 8th, 2020]
- 0015 Increased Awareness Of Low-t Helps Men Live Healthier Lives [Last Updated On: February 7th, 2025] [Originally Added On: June 9th, 2020]
- 0016 How Does Low-t Lead To Erectile Dysfunction? [Last Updated On: February 7th, 2025] [Originally Added On: June 10th, 2020]
- 0017 Testosterone Basics [Last Updated On: February 6th, 2025] [Originally Added On: June 11th, 2020]
- 0018 How Does Testosterone Impact Prostate Health? [Last Updated On: February 6th, 2025] [Originally Added On: June 12th, 2020]
- 0019 Testosterone And Other Sex Hormones Impact Asthma Response Dependent On Sex [Last Updated On: February 5th, 2025] [Originally Added On: June 13th, 2020]
- 0020 Recognizing Subtle Symptoms Of Testosterone Deficiency [Last Updated On: February 4th, 2025] [Originally Added On: June 15th, 2020]
- 0021 Testosterone Trivia [Last Updated On: February 4th, 2025] [Originally Added On: June 16th, 2020]
- 0022 The Health Benefits Of Testosterone And Sleep Are Interconnected [Last Updated On: February 3rd, 2025] [Originally Added On: June 17th, 2020]
- 0023 How Can I Restore My Testosterone Production Naturally? [Last Updated On: September 4th, 2025] [Originally Added On: June 18th, 2020]
- 0024 Low-t Quiz [Last Updated On: September 3rd, 2025] [Originally Added On: June 19th, 2020]
- 0025 Low Testosterone Might Mean Poor Sleep Need Testosterone Hormone Injections [Last Updated On: September 2nd, 2025] [Originally Added On: June 20th, 2020]
- 0026 Low Testosterone Contributes To Frailty With Age [Last Updated On: September 1st, 2025] [Originally Added On: June 21st, 2020]
- 0027 Japanese Testosterone Study Proves Physical And Psychological Benefits [Last Updated On: August 30th, 2025] [Originally Added On: June 23rd, 2020]
- 0028 Intramuscular Injections Are Safer Procedures [Last Updated On: August 29th, 2025] [Originally Added On: June 24th, 2020]
- 0029 Injecting Testosterone (im) [Last Updated On: October 24th, 2025] [Originally Added On: June 25th, 2020]
- 0030 Injectable Testosterone And Testosterone Cream [Last Updated On: February 14th, 2025] [Originally Added On: June 26th, 2020]
- 0031 Indiana Jones Vs. Rambo (hgh Testosterone) [Last Updated On: August 28th, 2025] [Originally Added On: June 27th, 2020]
- 0032 How Much Does Testosterone Control Men's Behavior? [Last Updated On: August 27th, 2025] [Originally Added On: June 28th, 2020]
- 0033 Getting To The Bottom Of Low-t Under-reported Sources Of Testosterone Deficiency [Last Updated On: February 14th, 2025] [Originally Added On: June 29th, 2020]
- 0034 How To Manage And Overcome Testosterone Deficiency [Last Updated On: August 26th, 2025] [Originally Added On: June 30th, 2020]
- 0035 Clomiphene Low-testosterone Andropause Treatment [Last Updated On: February 3rd, 2025] [Originally Added On: July 1st, 2020]
- 0036 How Do Synthetic Chemicals Impact Testosterone Secretion? [Last Updated On: August 18th, 2025] [Originally Added On: July 2nd, 2020]
- 0037 Interest In Bio-identical Testosterone Is Skyrocketing [Last Updated On: August 25th, 2025] [Originally Added On: July 3rd, 2020]
- 0038 Axiron Spray-application Testosterone Replacement Therapy [Last Updated On: August 24th, 2025] [Originally Added On: July 4th, 2020]
- 0039 Andropause: Male Menopause [Last Updated On: September 14th, 2025] [Originally Added On: July 5th, 2020]
- 0040 Testosterone Deficiency Treatment Options [Last Updated On: August 21st, 2025] [Originally Added On: July 6th, 2020]
- 0041 The Facts About Testosterone Hrt For Low-t [Last Updated On: August 22nd, 2025] [Originally Added On: July 7th, 2020]
- 0042 Misconceptions About Testosterone Replacement Therapy [Last Updated On: August 23rd, 2025] [Originally Added On: July 8th, 2020]
- 0043 Testosterone Replacement Therapy Facts And Myths [Last Updated On: October 4th, 2025] [Originally Added On: July 9th, 2020]
- 0044 Testosterone Injections For Testosterone Deficiency [Last Updated On: September 18th, 2022] [Originally Added On: July 10th, 2020]
- 0045 Testosterone Replacement Therapy May Help Aging Males Prevent Diabetes [Last Updated On: August 19th, 2025] [Originally Added On: July 11th, 2020]
- 0046 The Benefits Of Testosterone Replacement Therapy For Women [Last Updated On: August 17th, 2025] [Originally Added On: July 13th, 2020]
- 0047 How Can Testosterone Hrt Improve My Life Via Quality Low-t Treatments [Last Updated On: September 13th, 2025] [Originally Added On: July 14th, 2020]
- 0048 Frequently Asked Questions About Testosterone [Last Updated On: August 20th, 2025] [Originally Added On: July 15th, 2020]
- 0049 Bio-identical Testosterone Cypionate Injections [Last Updated On: August 16th, 2025] [Originally Added On: July 16th, 2020]
- 0050 All About Testosterone Creams [Last Updated On: August 13th, 2025] [Originally Added On: July 17th, 2020]
- 0051 Low Testosterone Treatment Protocols [Last Updated On: April 1st, 2025] [Originally Added On: July 19th, 2020]
- 0052 Testosterone Deficiency Drains Your Energy [Last Updated On: February 13th, 2025] [Originally Added On: July 21st, 2020]
- 0053 What Is Testosterone? [Last Updated On: August 11th, 2025] [Originally Added On: July 23rd, 2020]
- 0054 Eleven Signs Of Testosterone Deficiency [Last Updated On: March 30th, 2025] [Originally Added On: July 26th, 2020]
- 0055 Hypertension-Associated Cardiovascular Risks Increase Due To Both Low-T And High Testosterone [Last Updated On: February 18th, 2025] [Originally Added On: April 22nd, 2021]
- 0056 Everything to Know About Androgel [Last Updated On: March 27th, 2025] [Originally Added On: July 8th, 2021]
- 0057 Kinds of Testosterone Therapy – Which Is Right for You? [Last Updated On: March 21st, 2025] [Originally Added On: August 28th, 2021]
- 0058 This Study Says High Protein Diet May Suppress Testosterone Levels [Last Updated On: February 20th, 2025] [Originally Added On: March 28th, 2022]
- 0059 Testosterone and Estrogen Deficiency Associated With Increased Risk of Rotator Cuff Surgery [Last Updated On: February 14th, 2025] [Originally Added On: April 26th, 2022]
- 0060 Low Testosterone Accelerates Aging [Last Updated On: March 20th, 2025] [Originally Added On: May 3rd, 2022]
- 0061 Low Testosterone Endangers Your Health [Last Updated On: February 14th, 2025] [Originally Added On: May 14th, 2022]
- 0062 Testosterone Helps Modulate Immune Activity in the Digestive System [Last Updated On: February 14th, 2025] [Originally Added On: May 18th, 2022]
- 0063 Did you know: Testosterone treats depression! [Last Updated On: November 6th, 2025] [Originally Added On: May 19th, 2022]
- 0064 Benefits of Fenugreek – Boost Testosterone and More [Last Updated On: February 14th, 2025] [Originally Added On: May 23rd, 2022]
- 0065 Testicle Tanning: What is Tucker Carlson Talking About? [Last Updated On: April 16th, 2025] [Originally Added On: June 3rd, 2022]
- 0066 Using Testosterone to Combat Memory Issues in Diabetics [Last Updated On: February 14th, 2025] [Originally Added On: August 16th, 2022]
- 0067 About 40% of Men Have Low-T – and it Doubles the Risk of Severe COVID [Last Updated On: February 25th, 2025] [Originally Added On: September 21st, 2022]
- 0068 The Foods To Boost Your Testosterone…And The Foods To Avoid [Last Updated On: November 4th, 2025] [Originally Added On: September 30th, 2022]
- 0069 Tlando Testosterone: An Innovative Oral Therapy for Low-T [Last Updated On: November 3rd, 2025] [Originally Added On: October 1st, 2022]
- 0070 Testosterone Replacement Therapy (TRT) Explained [Last Updated On: April 8th, 2025] [Originally Added On: October 12th, 2022]
- 0071 Examining The Link Between Testosterone and Employability [Last Updated On: February 18th, 2025] [Originally Added On: November 8th, 2022]
- 0072 Standard Measure of Low Testosterone Doesn't Apply to Young Men [Last Updated On: March 12th, 2025] [Originally Added On: November 8th, 2022]
- 0073 Surprising Things that Cause Men’s Crashing Testosterone [Last Updated On: March 17th, 2025] [Originally Added On: January 5th, 2023]
- 0074 Understanding the Correlation between Testosterone Levels and Job Performance [Last Updated On: February 9th, 2025] [Originally Added On: February 9th, 2025]
- 0075 Link between Low Testosterone and Severe COVID Symptoms in Men [Last Updated On: February 12th, 2025] [Originally Added On: February 12th, 2025]
- 0076 The Good Job Grip: Is Testosterone the Key? [Last Updated On: February 13th, 2025] [Originally Added On: February 13th, 2025]
- 0077 Importance of Nutritional Balance in a Healthy Diet [Last Updated On: February 14th, 2025] [Originally Added On: February 14th, 2025]
- 0078 Invigorating Power of the Fenugreek Plant: A Natural Testosterone Energizer and More [Last Updated On: February 14th, 2025] [Originally Added On: February 14th, 2025]
- 0079 Unlocking the Testosterone Treasure: A Panacea for Cognitive Woes in Diabetic Patients [Last Updated On: February 14th, 2025] [Originally Added On: February 14th, 2025]
Word Count: 2456






